Spectrum of Magnetic Resonance Imaging Findings in Pancreatic and Other Abdominal Manifestations of Von Hippel-Lindau Disease in a Series of 23 patients: A Pictorial Review
Abstract
Context Von Hippel Lindau disease is a rare autosomal dominantly inherited multisystem disorder characterized by development of benign and malignant tumors. The abdominal manifestation of the syndrome are protean. Magnetic resonance plays an important role in identification of abdominal abnormalities and follow-up of lesions. Objective To describe magnetic resonance imaging findings and patterns of pancreatic and other principal abdominal manifestations in a series of von Hippel-Lindau (VHL) disease patients and to review literature. Methods We retrospectively reviewed abdominal magnetic resonance studies performed in 23 patients (10 males, 13 females) diagnosed of VHL. Results In all examined patients abdominal involvement was present. The pancreatic imaging findings detected were: unilocular cystic lesions (6/23: 26.1%); serous cystadenomas (11/23: 47.8%), including diffuse lesions (8/23: 34.8%); solid neuroendocrine tumors (8/23: 34.8%); cystic neuroendocrine tumors (1/23: 4.3%). The renal findings detected were: simple renal cysts (18/23: 78.3%); complex renal cysts (13/23: 56.5%), including benign lesions (10/23: 43.5%) and malignant lesions (3/23: 13.0%); renal carcinomas (11/23: 47.8%) and 5 of these (45.5%) were multiple and bilateral. Five patients (21.7%) presented pheochromocytoma (4 of these were bilateral; 80.0%) and 1 patient (4.3%) presented cystadenoma of the epididymis. Conclusions In VHL disease patients, magnetic resonance imaging plays an essential role in the identification of pancreatic and other abdominal lesions, in their follow-up, in the screening of asymptomatic gene carriers, and in their long-term surveillance.
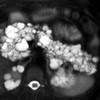
Image: Lobulated fluid cysts with a “bunch of grapes” pattern.
Downloads
References
Richard S, Graff J, Lindau J, Resche F. Von Hippel - Lindau disease. Lancet 2004; 363:1231-4.
Maher ER. Von Hippel - Lindau disease. Curr Mol Med 2004;4:833-42.
Taouli B, Ghouadni M, Corre´as JM, et al. Spectrum of abdominal imaging findings in von Hippel-Lindau disease. AJR Am J Roentgenol 2003;181(4):1049-1054.
Hes FJ, Feldberg MA. Von Hippel-Lindau disease: strategies in early detection (renal-, adrenal-, pancreatic masses). Eur Radiol 1999;9(4): 598-610.
Banks RE, Tirukonda P, Taylor C, et al.Genetic and epigenetic analysis of von HippeleLindau (VHL) gene alterations and relationship with clinical variables in sporadic renal cancer. Cancer Res 2006;66:2000-11.
Maher ER, Iselius L, Yates JR, Littler M, Benjamin C, Harris R, Sampson J, Williams A, Ferguson-Smith MA, Morton N. Von Hippel-Lindau disease: a genetic study. J Med Genet 1991;28:443-447.
Seizinger BR, Rouleau GA, Ozelius LJ, et al. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma.Nature 1988;332(6161):268-269.
Latif F, Tory K, Gnarra J, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science 1993;260(5112):1317-1320.
Choyke PL, Glenn GM, Walther MM, et al. Von Hippel-Lindau disease: genetic, clinical, and imaging features. Radiology 1995;194(3):629-642.
Kaelin WG, Iliopoulos O, Lonergan KM, Ohh M. Functions of the von Hippel-Lindau tumour suppressor protein. J Intern Med 1995; 243:535-539.
Karsdorp N, Elderson A, Wittebol-Post D, et al. Von Hippel-Lindau disease: new strategies in early detection and treatment. Am J Med 1994;97(2): 158-168.
Melmon KL, Rosen SW. Lindau’s disease: review of the literature and study of a large kindred. Am J Med1964;36:595-617.
Patard JJ, Rodriguez A, Rioux-Leclercq N, et al. Prognostic significance of the mode of detection in renal tumours. BJU Int 2002;90:358-63.
Friedrich CA.Von Hippel-Lindau syndrome: a pleomorphic condition. Cancer 1999;86(11 suppl):2478-2482.
Leung RS, Biswas SV, Duncan M, Rankin S. Imaging features of von Hippel-Lindau disease. Radiographics 2008; Jan-Feb 28(1):65-79.
Tattersall DJ, Moore NR. Von Hippel-Lindau disease: MRI of abdominal manifestations. Clin Radiol 2002;57:85-92.
Neumann HP, Dinkel E, Brambs H, et al. Pancreatic lesions in the von Hippel-Lindau syndrome. Gastroenterology 1991; 101(2): 465-471.
Maher ER, Yates JRW, Harries R, et al. Clinical features and natural history of von Hippel-Lindau disease. Q J Med 1990;77:1151-63.
Agrawal D, Maimone SS, Wong RC, Isenberg G, Faulx A, Chak A. Prevalence and clinical significance of pancreatic cysts associated with cysts in other organs. Dig Liver Dis 2011; Oct 43(10):797-801.
Hough DM, Stephens DH, Johnson CD, Binkovitz LA. Pancreatic lesions in von Hippel-Lindau disease: prevalence, clinical significance, and CT findings. AJR Am J Roentgenol 1994; 162(5): 1091-1094.
Torreggiani WC, Keogh C, Ismail KA, Munk PL, Nicolau S. Von Hippel-Lindau disease: a radiological essay. Clin Radiol 2002;57:670-680.
Agarwal N, Kumar S, Dass J, Arora VK, Rathi V. Diffuse pancreatic serous cystadenoma associated with neuroendocrine carcinoma: a case report and review of literature. JOP 2009; Jan 8 10(1):55-8. Review.
Kanno A, Satoh K, Hamada S, Hirota M, Masamune A, Motoi F, Egawa S, Unno M, Ishida K, Kimura K, Shuin T, Shimosegawa T. Serous cystic neoplasms of the whole pancreas in a patient with von Hippel-Lindau disease. Intern Med. 2011;50(12):1293-8.
Marcos HB, Libutti SK, Alexander HR, Lubensky IA, Bartlett DL, Walther MM. Neuroendocrine tumors of the pancreas in von Hippel-Lindau disease. Spectrum of appearances at CT and MR imaging with histopathologic comparison. Radiology 2002;225:751-758.
Tamura K, Nishimori I, Ito T, Yamasaki I, Igarashi H, Shuin T. Diagnosis and management of pancreatic neuroendocrine tumor in von Hippel-Lindau disease. World J Gastroenterol 2010; Sep 28 16(36):4515-8.
Binkovitz LA, Johnson CD, Stephens DH. Islet cell tumors in von Hippel-Lindau disease: increased prevalence and relationship to the multiple endocrine neoplasias. AJR Am J Roentgenol 1990; Sep 155(3):501-5.
Lubensky IA, Pack S, Ault D. et al. Multiple neuroendocrine tumors of the pancreas in von Hippel-Lindau disease patients: histopathological and molecular genetic analysis. Am J Pathol 1998;153:223-231.
Hammel PR, Vilgrain V, Terris B, Penfornis A, et al. Pancreatic involvement in von Hippel- Lindau disease. The Groupe Francophone d’ etude de la Maladie de Von Hippel- Lindau.Gastroenterology 2000;119:1087-1095.
Delman KA, Shapiro SE, Jonasch EW, Lee JE, Curley SA, Evans DB, Perrier ND. Abdominal visceral lesions in von Hippel-Lindau disease: incidence and clinical behavior of pancreatic and adrenal lesions at a single center. World J Surg 2006; May 30(5):665-9.
Yamasaki I, Nishimori I, Ashida S, Kohsaki T. et al. Clinical characteristic of pancreatic neuroendocrine tumors in Japanese patients with von Hippel- Lindau disease. Pancreas 2006;33:382-385.
Libutti SK, Choyke PL, Alexander HR, et al. Clinical and genetic analysis of patients with pancreatic neuroendocrine tumors associated with von Hippel-Lindau disease. Surgery 2000;128:1022-1027.
Libutti SK, Choyke PL, Bartlett DL, et al. Pancreatic neuroendocrine tumors associated with von Hippel-Lindau disease: diagnostic and management recommendations. Surgery 1998;124:1153-1159.
Blansfield JA, Choyke L, Morita SY, Choyke PL, Pingpank JF, Alexander HR, Seidel G, Shutack Y, Yuldasheva N, Eugeni M, Bartlett DL, Glenn GM, Middelton L, Linehan WM, Libutti SK. Clinical, genetic and radiographic analysis of 108 patients with von Hippel-Lindau disease (VHL) manifested by pancreatic neuroendocrine neoplasms (PNETs). Surgery 2007;142(6):814-818;discussion 818.e1-2.
Neuzillet C, Vullierme MP, Couvelard A, Sauvanet A, Levy P, Richard S, Ruszniewski P, Hammel P. Difficult diagnosis of atypical cystic pancreatic lesions in von Hippel-Lindau disease. J Comput Assist Tomogr 2010;34(1):140-5.
Plöckinger U, Rindi G, Arnold R, Eriksson B, Krenning EP,de Herder WW, Goede A, Caplin M, Oberg K, Reubi JC,Nilsson O, Delle Fave G, Ruszniewski P, Ahlman H, Wiedenmann B. Guidelines for the diagnosis and treatment of neuroendocrine gastrointestinal tumours. A consensus statement on behalf of the European Neuroendocrine Tumour Society (ENETS). Neuroendocrinology 2004; 80:394-424.
Maeda H, Nishimori I, Okabayashi T Kohsaki T,et al.Total pancreatectomyfor multiple neuroendocrine tumors of the pancreas in a patient with von Hippel-Lindau disease.Clin J Gastroenterol 2009;2:222-225.
Corleto VD, Cotesta D, Petramala L, Panzuto F, Pagnini C, Masoni L, Verrienti A, Delle Fave G, Filetti S, Letizia C. Late recurrence after surgical resection of a pancreatic tumor in von Hippel-Lindau disease. JOP 2009;4 10(5):562-5.
Meister M, Choyke P, Anderson C, Patel U. Radiological evaluation, management, and surveillance of renal masses in Von Hippel-Lindau disease. Clin Radiol 2009; Jun 64(6):589-600.
Choyke PL, Glenn GM, Walther MM, et al. The natural history of renal lesions in von Hippel-Lindau disease: a serial CT study in 28 patients. AJR Am J Roentgenol 1992;159(6):1229-1234.
Olea I, Vargas B, Sobrino B, Domínguez E. Abdominal manifestations in von Hippel-Lindau disease in a group of 7 patients and literature review. Radiologia 2009; Mar-Apr 51(2):198-203.
Choyke PL, Glenn GM, Walther MM, et al. Hereditary renal cancers. Radiology 2003;226:33-46.
Malek RS, Omess PJ, Benson RC Jr, Zincke H. Renal cell carcinoma in von Hippel-Lindau syndrome. Am J Med 1987;82(2):236-238.
Walther MM, Lubensky IA, Venzon D, et al. Prevalence of microscopic lesions in grossly normal renal parenchyma from patients with von Hippel-Lindau disease, sporadic renal cell carcinoma and no renal disease: clinical implications. J Urol 1995;154:2010-2014.
Ogawa O, Kakehi Y, Ogawa K, Koshiba M, Sugiyama T, Yoshida O. Allelic loss at chromosome 3p characterizes clear cell phenotype of renal cell carcinoma. Cancer Res 1991; 51:949-953.
Walther MM, Choyke PL, Glenn G, et al. Renal cancer in families with hereditary renal cancer: prospective analysis of a tumor size threshold for renal parenchymal sparing surgery. J Urol 1999; 161:1475-1479.
Herring JC, Enquist EG, Chernoff A, Linehan WM, Choyke PL, Walther MM, (2001) Parenchymal sparing surgery in patients with hereditary renal cell carcinoma: 10-year experience. J Urol,165:777-781.
Gervais DA, Arellano RS, Mueller PR. Percutaneous radiofrequency ablation of renal cell carcinoma. Eur Radiol 2001; 15(5): 960-967.
Choyke PL, Filling-Katz MR, Shawker TH, et al. Von Hippel-Lindau disease: radiologic screening for visceral manifestations. Radiology 1990;174: 815-820.
Rao AB, Koeller KK, Adair CF. From the archives of the AFIP. Paragangliomas of the head and neck: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics 1999;19(6):1605-32.
Blake MA, Kalra MK, Maher MM. et al, (2004) Pheochromocytoma: An Imaging Chameleon. Radiographics,24:S87-S99.
Olsen WL, Dillon WP, Kelly WM, et al. MR imaging of paragangliomas. AJR 2004;148:201-204.
Lee KY, Oh YW, Noh HJ, et al. Extraadrenal Paragangliomas of the Body: Imaging Features. AJR 2006;187:492-504.
Woodward PJ, Schwab CM, Sesterhenn IA. From the archives of the AFIP: extratesticular scrotal masses: radiologic-pathologic correlation. Radiographics 2003;23(1):215-40. Review.
Smirnitopoulos JG, Lonergan GJ, Abbott RM. et al. Image interpretation Session: 1998. Radiographics 1999;19(1):205-233
Peyrì Reye E, Casalotos Serramia J. Cistoadenoma papilar de epidìdimo. Actas Urologicas Espanola 2000;761-763
Akbar SA, Sayyed TA, Jafri SZ, Hasteh F, Neill JS. Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics 2003;23(6):1461-76.
Leung ML, Gooding GA, Williams RD. High-resolution sonography of scrotal contents in asymptomatic subjects. AJR Am J Roentgenol 1984;143(1):161-4.
Kim W, Rosen MA, Langer JE, Banner MP, Siegelman ES, Ramchandani P. US-MR Imaging correlation in pathologic conditions of the scrotum. Radiographics 2007;27(5):1239-53.
Funk KC, Heiken JP. Papillary Cystadenoma of the Broad Ligament in a Patient with von Hippel-Lindau Disease. AJR 1989; 153:527-528.
Copyright (c) 2014 Rossella Graziani, Simona Mautone, Mario Vigo, Riccardo Manfredi, Giuseppe Opocher, Massimo Falconi

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.