Natural History of Branch-Duct Intraductal Papillary Mucinous Neoplasms of the Pancreas: A Case Report
Abstract
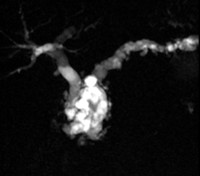
Context The natural history of incidental branch-duct intraductal papillary mucinous neoplasm of the pancreas is still unknown. Case report The case of a 74-year-old man who had been diagnosed 14 years previously with an incidental branch-duct intraductal papillary mucinous neoplasm of the pancreatic head, 30 mm in size, without mural nodules and dilatation of the main pancreatic duct is herein reported. After an exploratory laparotomy at the time of diagnosis (when he was 60 year-old), the patient was enrolled in a surveillance program. Fourteen years after the diagnosis, the cystic lesion showed an increase in size, Wirsung duct dilatation and the presence of several mural nodules. A total pancreatectomy was performed and a diagnosis of mixed-intraductal papillary mucinous neoplasm diffused throughout the entire pancreas with high grade dysplasia, and a micro-invasive carcinoma (<1 mm) of the pancreatic head was reached. Conclusion The present case confirmed that the natural history of branch-duct intraductal papillary mucinous neoplasms is unpredictable. Thus, an appropriate surveillance program is required for prompt identification of the signs predictive of a malignant transformation of branch-duct intraductal papillary mucinous neoplasms. In high-volume centers, surgery should seriously be considered in young patients who are fit for surgery.
Image: MRI plus cholangiopancreatography.
Downloads
References
Furukawa T, Klöppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, Hruban RH, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch 2005; 447: 794-799. [PMID:16088402]
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, Yamaguchi K, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 2006; 6: 17-32. [PMID:16327281]
Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12: 183-197. [PMID:22687371]
Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, Friess H, et al. European expert consensus statement on cystic tumours of the pancreas. Dig Liver Dis 2013; 45: 703-711. [PMID:23415799]
Sahora K, Mino-Kenudson M, Brugge W, Thayer SP, Ferrone CR, Sahani D, Pitman MB, et al. Branch duct intraductal papillary mucinous neoplasms: does cyst size change the tip of the scale? A critical analysis of the revised international consensus guidelines in a large single-institutional series. Ann Surg. 2013; 258: 466-475. [PMID:24022439]
Anand N, Sampath K, Wu BU. Cyst features and risk of malignancy in intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Clin Gastroenterol Hepatol. 2013; 11: 913-921. [PMID:23416279]
Correa-Gallego C, Do R, Lafemina J, Gonen M, D'Angelica MI, DeMatteo RP, Fong Y, et al. Predicting dysplasia and invasive carcinoma in intraductal papillary mucinous neoplasms of the pancreas: development of a preoperative normogram. Ann Surg Oncol. 2013; 20: 4348-4355. [PMID:24046103]
Kim KW, Park SH, Pyo J, Yoon SH, Byun JH, Lee MG, Krajewski KM, et al. Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas. A meta-analysis. Ann Surg. 2014; 259: 72-81. [PMID:23657084]
Fritz S, Klauss M, Bergmann F, Hackert T, Hartwig W, Strobel O, Bundy BD, et al. Small (Sendai negative) branch-duct IPMNs: not harmless. Ann Surg. 2012; 256: 313-320. [PMID:22791105]
Tanno S, Nakano Y, Nishikawa T, Nakamura K, Sasajima J, Minoguchi M, Mizukami Y, et al. Natural history of branch duct intraductal papillary-mucinous neoplasms of the pancreas without mural nodules: long-term follow-up results. Gut. 2008; 57: 339-343. [PMID:17660227]
Copyright (c) 2014 Riccardo Casadei, Claudio Ricci, Marielda D’Ambra, Giovanni Taffurelli, Caterina C Zingaretti, Carlo A Pacilio, Lucia Calculli, Nico Pagano, Francesco Minni

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.