Non-Functioning Pancreatic Neuroendocrine Tumor Accompanied with Multiple Liver Metastases: Remorseful Case and Literature Review
Abstract
Context Pancreatic neuroendocrine tumor (P-NET) is a rare and slow-growing tumor. Unfortunately, there is no clear consensus on the role and timing of surgery for primary tumor and liver metastases, although current reports refer to liver surgery including LT for unresectable liver metastases. Case report A thirty-nine-year-old man was diagnosed with nonfunctioning pancreatic neuroendocrine tumor (P-NET) in the pancreatic head, with multiple liver metastases. The tumor was 2.5 cm in diameter and he was asymptomatic. Small but multiple metastases were detected in the liver, and no extrahepatic metastases were observed. We initially intended to control the liver metastases before resection of the primary tumor. To begin with, transarterial chemoembolization (TACE) and transcatheter arterial infusion (TAI) were repeated. Thereafter, systemic chemotherapy and biotherapy were introduced according to follow-up assessments. Unfortunately, imaging assessment at about 10 months later revealed that liver metastases were partially enlarged, although some were successfully treated. Therefore, these therapies were switched to other regimens, and TACE/TAI, systemic chemotherapies and biotherapies were repeated. Although liver metastases seemed to be stable for a while, the primary tumor was enlarged even after therapy. At 3.5 years after initial diagnosis, the primary tumor became symptomatic (pain and jaundice). Liver metastases enlarged and massive swelling of the para-aortic lymph nodes was observed. Thereafter, palliative therapy was the main course of action. He died at 4.3 years after initial diagnosis. Conclusion Our young patient could have been a candidate for initial surgery for primary tumor and might have had a chance of subsequent liver transplantation for unresectable metastases. Surgeons still face questions in deciding the best surgical scenario in patients with P-NET with liver metastases.
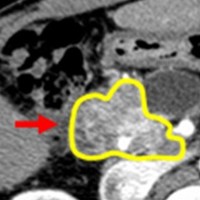
Image: Primary tumor grew after therapy.
Downloads
References
Kimura W, Tezuka K, Hirai I. Surgical management of pancreatic neuroendocrine tumors. Surg Today 2011; 41: 1332-43. [PMID: 21922354]
International Union Against Cancer (UICC). TNM classification of malignant tumors. 7th ed. Oxford: Wiley-Blackwell, 2009.
Heitz P, Komminoth P, Perren A, Klimstra D, Dayal Y. Tumors of the endocrine pancreas. In: De Lellis R, Lloyd R, Heitz P, Eng C, eds. World Health Organization classification of tumors: pathology and genetics of tumors of endocrine organs. 1st ed. Lyon: IARC Press, 2004: 177-82.
Bettini R, Mantovani W, Boninsegna L, Crippa S, Capelli P, Bassi C, et al. Primary tumour resection in metastatic nonfunctioning pancreatic endocrine carcinomas. Dig Liver Dis 2009; 41: 49-55. [PMID: 18463008]
Bloomston M, Muscarella P, Shah MH, Frankel WL, Al-Saif O, Martin EW, et al. Cytoreduction results in high perioperative mortality and decreased survival in patients undergoing pancreatectomy for neuroendocrine tumors of the pancreas. J Gastrointest Surg 2006; 10: 1361-70. [PMID: 17175455]
Hanazaki K, Sakurai A, Munekage M, Ichikawa K, Namikawa T, Okabayashi T, et al. Surgery for a gastroenteropancreatic neuroendocrine tumor (GEPNET) in multiple endocrine neoplasia type 1. Surg Today 2013; 43: 229-36. [PMID: 23076685]
Touzios JG, Kiely JM, Pitt SC, Rilling WS, Quebbeman EJ, Wilson SD, et al. Neuroendocrine hepatic metastases: does aggressive management improve survival? Ann Surg 2005; 241: 776-83. [PMID: 15849513]
Norton JA, Warren RS, Kelly MG, Zuraek MB, Jensen RT. Aggressive surgery for metastatic liver neuroendocrine tumors. Surgery 2003; 134: 1057-63. [PMID: 14668741]
Mayo SC, de Jong MC, Pulitano C, Clary BM, Reddy SK, Gamblin TC, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol 2010; 17: 3129-36. [PMID: 20585879]
Chapman WC. Liver transplantation for unresectable metastases to the liver: a new era in transplantation or a time for caution? Ann Surg 2013; 257: 816-7. [PMID: 23532106]
Shibata C, Egawa S, Motoi F, Morikawa T, Naitoh T, Unno M, et al. Surgery for pancreatic neuroendocrine tumors. Nihon Geka Gakkai zasshi 2012; 113: 502-6. [PMID: 23330458]
Kouvaraki MA, Shapiro SE, Cote GJ, Lee JE, Yao JC, Waguespack SG, et al. Management of pancreatic endocrine tumors in multiple endocrine neoplasia type 1. World J Surg 2006; 30: 643-53. [PMID: 16680581]
Patel KK, Kim MK. Neuroendocrine tumors of the pancreas: endoscopic diagnosis. Curr Opin Gastroenterol 2008; 24: 638-42. [PMID: 19122508]
Figueiredo FA, Giovannini M, Monges G, Bories E, Pesenti C, Caillol F, et al. EUS-FNA predicts 5-year survival in pancreatic endocrine tumors. Gastrointest Endosc 2009; 70: 907-14. [PMID: 19640525]
Chatzipantelis P, Konstantinou P, Kaklamanos M, Apostolou G, Salla C. The role of cytomorphology and proliferative activity in predicting biologic behavior of pancreatic neuroendocrine tumors: a study by endoscopic ultrasound-guided fine-needle aspiration cytology. Cancer 2009; 117: 211-6. [PMID: 19350669]
McEntee GP, Nagorney DM, Kvols LK, Moertel CG, Grant CS. Cytoreductive hepatic surgery for neuroendocrine tumors. Surgery 1990; 108: 1091-6. [PMID: 1701060]
Thompson NW. Current concepts in the surgical management of multiple endocrine neoplasia type 1 pancreatic-duodenal disease. Results in the treatment of 40 patients with Zollinger-Ellison syndrome, hypoglycaemia or both. J Intern Med 1998; 243: 495-500. [PMID: 9681848]
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334: 693-9. [PMID: 8594428]
Gottwald T, Koveker G, Busing M, Lauchart W, Becker HD. Diagnosis and management of metastatic gastrinoma by multimodality treatment including liver transplantation: report of a case. Surg Today 1998; 28: 551-8. [PMID: 9607910]
Le Treut YP, Grégoire E, Klempnauer J, Belghiti J, Jouve E, Lerut J, et al; For ELITA. Liver transplantation for neuroendocrine tumors in Europe-results and trends in patient selection: a 213-case European liver transplant registry study. Ann Surg 2013; 257: 807-15. [PMID: 23532105]
Mazzaferro V, Pulvirenti A, Coppa J. Neuroendocrine tumors metastatic to the liver: how to select patients for liver transplantation? J Hepatol 2007; 47: 460-6. [PMID: 17697723]
de Herder WW, Mazzaferro V, Tavecchio L, Wiedenmann B. Multidisciplinary approach for the treatment of neuroendocrine tumors. Tumori 2010; 96: 833-46. [PMID: 21302641]
Alessiani M, Tzakis A, Todo S, Demetris AJ, Fung JJ, Starzl TE. Assessment of five-year experience with abdominal organ cluster transplantation. J Am Coll Surg 1995; 180: 1-9. [PMID: 8000645]
Pavel M, Baudin E, Couvelard A, Krenning E, Öberg K, Steinmüller T, et al; Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2012; 95: 157-76. [PMID: 22262022]
Pascher A, Klupp J, Neuhaus P. Endocrine tumours of the gastrointestinal tract. Transplantation in the management of metastatic endocrine tumours. Best Pract Res Clin Gastroenterol 2005; 19: 637-48. [PMID: 16183532]
Gregoire E, Le Treut YP. Liver transplantation for primary or secondary endocrine tumors. Transpl Int 2010; 23: 704-11. [PMID: 20492617]
Bonaccorsi-Riani E, Apestegui C, Jouret-Mourin A, Sempoux C, Goffette P, Ciccarelli O, et al. Liver transplantation and neuroendocrine tumors: lessons from a single centre experience and from the literature review. Transpl Int 2010; 23: 668-78. [PMID: 20478000]
Rosenau J, Bahr MJ, von Wasielewski R, Mengel M, Schmidt HH, Nashan B, et al. Ki67, E-cadherin, and p53 as prognostic indicators of long-term outcome after liver transplantation for metastatic neuroendocrine tumors. Transplantation 2002; 73: 386-94. [PMID: 11884935]
Copyright (c) 2014 Tomohide Hori, Kyoichi Takaori, Michiya Kawaguchi, Kohei Ogawa, Toshihiko Masui, Takamichi Ishii, Hiromitsu Nagata, Masato Narita, Yuzo Kodama, Norimitsu Uza, Shinji Uemoto

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.