Inoperable Pancreatic Cancer Patients Who Have Prolonged Survival Exhibit an Increased Risk of Cholangitis
Abstract
Context Endoscopically placed metal stents, which are patent for 4-9 months, have been the favored decompressive strategy for biliary obstruction due to inoperable pancreatic cancer in order to minimize interventions. However, in the past decade chemotherapeutic options have improved survival. This raises the question of whether metal stents will continue to be the optimal method of decompression. Objective We performed a study to determine the outcome of patients with non-operatively managed pancreatic adenocarcinoma with regards to the development of cholangitis. Design We reviewed all ERCP performed for malignant distal biliary obstruction in between December 1999 and December 2005 at University of California, San Francisco (UCSF). Patients Only patients who received chemotherapy for pancreatic adenocarcinoma were included. Patients who underwent surgical biliary diversion procedures were excluded. Primary outcome measurement The primary outcome was the development of cholangitis requiring hospitalization. Results Among 200 patients with malignant distal biliary obstruction who underwent endoscopic biliary decompression procedures, 54 met study criterion. Metal stents were employed in 90.7% of these cases. The median survival of this population was 12.7 months (range: 2.6-34.6 months). Only 3 of 26 patients (11.5%) surviving one year or less developed cholangitis compared to 13 of 28 (46.5%) who survived more than one year. Thus patients surviving greater than one year had a five fold increase in the odds of developing cholangitis (odds ratio: 4.92; P=0.017). Conclusions This cohort of inoperable pancreatic cancer patients undergoing chemotherapy survived longer than the expected patent period of metal stents employed for biliary decompression. The occurrence of cholangitis requiring hospitalization does increase markedly among long term survivors.
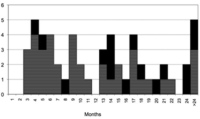
Image: Number of patients who survived.
Downloads
References
Hochster HS, Haller DG, de Gramont A, et al. Consensus report of the international society of gastrointestinal oncology on therapeutic progress in advanced pancreatic cancer. Cancer 2006; 107:676-85. [PMID 16847885]
Burris HA, 3rd, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 1997; 15:2403-13. [PMID 9196156]
Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 2007; 25:1960-6. [PMID 17452677]
Tempero M, Plunkett W, Ruiz Van Haperen V, et al. Randomized phase II comparison of dose-intense gemcitabine: thirty-minute infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J Clin Oncol 2003; 21:3402-8. [PMID 12885837]
Ko AH, Quivey JM, Venook AP, et al. A phase II study of fixed-dose rate gemcitabine plus low-dose cisplatin followed by consolidative chemoradiation for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys 2007; 68:809-16. [PMID 17363191]
Moss AC, Morris E, Mac Mathuna P. Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev 2006:CD004200. [PMID 16625598]
Speer AG, Cotton PB, Russell RC, et al. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 1987; 2:57-62. [PMID 2439854]
Smith AC, Dowsett JF, Russell RC, et al. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet 1994; 344:1655-60. [PMID 7996958]
Artifon EL, Sakai P, Cunha JE, Dupont A, Filho FM, Hondo FY, et al. Surgery or endoscopy for palliation of biliary obstruction due to metastatic pancreatic cancer. Am J Gastroenterol 2006; 101:2031-7. [PMID 16968509]
Prat F, Chapat O, Ducot B, et al. A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. Gastrointest Endosc 1998; 47:1-7. [PMID 9468416]
Davids PH, Groen AK, Rauws EA, et al. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet 1992; 340:1488-92. [PMID 1281903]
Carr-Locke DL, Ball, TJ, Connors, PJ, et al. Multicenter, randomized trial of wallstent biliary endoprosthesis versus plastic stent. Gastrointest Endosc 1993; 3 9:310.
Knyrim K, Wagner HJ, Pausch J, et al. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy 1993; 25:207-12. [PMID 8519239]
Kaassis M, Boyer J, Dumas R, et al. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc 2003; 57:178-82. [PMID 12556780]
Prat F, Chapat O, Ducot B, et al. Predictive factors for survival of patients with inoperable malignant distal biliary strictures: a practical management guideline. Gut 1998; 42:76-80. [PMID 9505889]
Lee JG. Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol 2009; 6:533-541. [PMID 21207254]
Isayama H, Komatsu Y, Tsujino T, et al. A prospective randomised study of ''covered'' versus ''uncovered'' diamond stents for the management of distal malignant biliary obstruction. Gut 2004; 53:729-34. [PMID 15082593]
Soderlund C, Linder S. Covered metal versus plastic stents for malignant common bile duct stenosis: a prospective, randomized, controlled trial. Gastrointest Endosc 2006; 63:986-95. [PMID 16733114]
O'Brien S, Hatfield AR, Craig PI, et al. A three year follow up of self expanding metal stents in the endoscopic palliation of longterm survivors with malignant biliary obstruction. Gut 1995; 36:618-21. [PMID 7537708]
Yoon WJ, Lee JK, Lee KH, et al. A comparison of covered and uncovered Wallstents for the management of distal malignant biliary obstruction. Gastrointest Endosc 2006; 63:996-1000. [PMID 16733115]
Takasawa O, Fujita N, Kobayashi G, et al. Endoscopic biliary drainage for patients with unresectable pancreatic cancer with obstructive jaundice who are to undergo gemcitabine chemotherapy. World J Gastroenterol 2006; 12:7299-303. [PMID 17143944]
Maire F, Hammel P, Ponsot P, Aubert A, O'Toole D, Hentic O, et al. Long-term outcome of biliary and duodenal stents in palliative treatment of patients with unresectable adenocarcinoma of the head of pancreas. Am J Gastroenterol 2006; 101:735-42. [PMID 16635221]
Levy P HP, O'Toole D, Tigaud J, et al. Survival of patients with non-resectable pancreatic ductal adenocarcinoma: published data is rendered obsolete with new therapeutic strategies. Gastroenterology 2002; 122:A-567.
Saif MW. Pancreatic cancer: is this bleak landscape finally changing? Highlights from the '43rd ASCO Annual Meeting'. Chicago, IL, USA. June 1-5, 2007. JOP. J Pancreas (Online) 2007; 8:365-73. [PMID 17625289]
Tham TC, Carr-Locke DL, Vandervoort J, et al. Management of occluded biliary Wallstents. Gut 1998; 42:703-7. [PMID 9659168]
Bueno JT, Gerdes H, Kurtz RC. Endoscopic management of occluded biliary Wallstents: a cancer center experience. Gastrointest Endosc 2003; 58:879-84. [PMID 14652557]
Familiari P, Bulajic M, Mutignani M, et al. Endoscopic removal of malfunctioning biliary self-expandable metallic stents. Gastrointest Endosc 2005; 62:903-10. [PMID 16301035]
Speer AG, Cotton PB, Rode J, Seddon AM, Neal CR, Holton J, Costerton JW. Biliary stent blockage with bacterial biofilm. A light and electron microscopy study. Ann Intern Med 1988; 108:546-53. [PMID 2450501]
Valiozis I, Zekry A, Williams SJ, et al. Palliation of hilar biliary obstruction from colorectal metastases by endoscopic stent insertion. Gastrointest Endosc 2000; 51:412-7. [PMID 10744811]
Meyerhardt JA, Mayer RJ. Systemic therapy for colorectal cancer. N Engl J Med 2005; 352:476-87. [PMID 15689586]
Odemis B, Parlak E, Basar O, et al. Biliary tract obstruction secondary to malignant lymphoma: experience at a referral center. Dig Dis Sci 2007; 52:2323-32. [PMID 17406815]
Farrell J, Elsaleh H, Garcia, et al. Human equilibrative nucleoside transporter 1 levels predict response to gemcitabine in patients with pancreatic cancer. Gastroenterology 2009; 136:187-195. [PMID 18992248]
Leung J, Rahim N. The role of covered self-expandable metallic stents in malignant biliary strictures. Gastrointest Endosc 2006; 63:1001-3. [PMID 16733116]
Copyright (c) 2011 James L Buxbaum, Scott W Biggins, Karen C Bagatelos, John M Inadomi, James W Ostroff

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.