Pancreatic Cyst Aspirate CEA Levels: Two's the Charm
Abstract
Context Pancreatic cysts are increasingly detected incidentally, many of which are premalignant. Despite EUS-FNA and CEA level measurement, the diagnosis of a premalignant cyst may remain uncertain. Case report We report two cases of incidentally found pancreatic cysts where initial EUS-FNA cyst aspirates yielded thin fluid with very low CEA levels. Repeat aspirations one year later revealed markedly different results (slightly viscous fluid with significantly elevated CEA levels) which prompted surgical resection in both cases. Final surgical pathology revealed mucinous cystic neoplasms. Conclusion Pancreatic cyst fluid CEA levels may increase over time, possibly due to neoplastic progression. A heightened index of suspicion for a neoplastic cyst should remain in the appropriate patient population, despite conflicting data. In cases of initial low aspirate CEA levels, we recommend a repeat EUS-FNA at a later date to exclude a premalignant lesion.
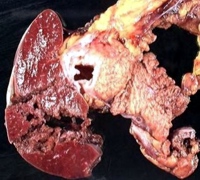
Image: Resected mucinous cystic neoplasm.
Downloads
References
Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C, Warshaw AL. Cystic neoplasms of the pancreas. N Engl J Med 2004; 351:1218-26. [PMID 15371579]
Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg 2004; 239:651-7. [PMID 15082969]
Fernández-del Castillo C, Targarona J, Thayer SP, Rattner DW, Brugge WR, Warshaw AL. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg 2003; 138:427-3. [PMID 12686529]
Brugge WR. Evaluation of pancreatic cystic lesions with EUS. Gastrointest Endosc 2004; 59:698-707. [PMID 15114319]
Ahmad NA, Kochman ML, Lewis JD, Ginsberg GG. Can EUS alone differentiate between malignant and benign cystic lesions of the pancreas? Am J Gastroenterol 2001; 96:3295-300. [PMID 11774939]
Ahmad NA, Kochman ML, Brensinger C, Brugge WR, Faigel DO, Gress FG et al. Interobserver agreement among endosonographers for the diagnosis of neoplastic versus non-neoplastic pancreatic cystic lesions. Gastrointest Endosc 2003; 58:59-64. [PMID 12838222]
Brugge WR, Lewandrowski K, Lee-Lewandrowski E, Centeno BA, Szydlo T, Regan S, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology 2004; 126:330-6. [PMID 15131794]
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 2006; 6:17-32. [PMID 16327281]
Reddy RP, Smyrk TC, Zapiach M, Levy MJ, Pearson RK, Clain JE, et al. Pancreatic mucinous cystic neoplasm defined by ovarian stroma: demographics, clinical features, and prevalence of cancer. Clin Gastroenterol Hepatol 2004; 2:1026-31. [PMID 15551256]
Khalid A, Brugge W. ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cysts. Am J Gastroenterol 2007; 102:2339-49. [PMID 17764489]
Crippa S, Salvia R, Warshaw AL, Domínguez I, Bassi C, Falconi M, et al. Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Ann Surg 2008; 247:571-9. [PMID 18362619]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, et al. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J Surg Pathol 1999. 23:410-22. [PMID 10199470]
Copyright (c) 2011 John Y Nasr, Kevin McGrath

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.