The Natural History of a Branch Duct Intraductal Papillary Mucinous Neoplasm in a Patient with Lady Windermere Syndrome: A CASE REPORTS
Abstract
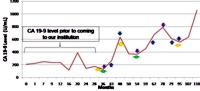
Context "Low-risk" branch duct intraductal papillary mucinous neoplasm (IPMN) is defined as pancreatic epithelial cellular proliferation of small branch ducts that lack malignant characteristics. At present, our understanding of the natural history of "low-risk" branch duct IPMN is still evolving. Lady Windermere syndrome is a disorder seen in non-smoking women with no pre-existing pulmonary disease affecting the lingula and/or right middle lobe with Mycobacterium avium-intracellulare complex. We present a case with pancreatic adenocarcinoma after a six-year surveillance of "low-risk" branch duct IPMN in an asymptomatic elderly white woman with Lady Windermere syndrome. Case report A 79-year-old woman was referred to our institution because of pancreatic cystic abnormalities and elevated carbohydrate antigen 19-9 (CA 19-9). While at our institution, she was also diagnosed with Lady Windermere syndrome. Multiple abdominal imaging studies, endoscopic retrograde cholangiopancreatography, computer tomography, and magnetic resonance cholangiopancreatography (MRCP) were performed in the ensuing 6 years, all consistent with "low-risk" branch duct IPMN. No progression was seen until year 6 when MRCP showed a 2 cm pancreatic cancer. Because of multiple comorbidities, the patient chose chemotherapy over a pancreaticoduodenectomy. She developed respiratory failure and died after one cycle of gemcitabine. Conclusions "Low-risk" branch duct IPMN may be a heterogeneous disease in which some cases can transform into malignant pancreatic neoplasms despite the absence of the so-called "high risk" features on imaging studies. Clinical management, therefore, requires individualized flexibility. In addition, when there is coexistence of Lady Windermere syndrome and pancreatic cancer, prompt diagnosis and treatment of Lady Windermere syndrome should be considered prior to chemoradiotherapy or surgery.
Image: CA 19-9 level during follow-up of "low-risk" branch-duct IPMN.
Downloads
References
Longnecker DS, Adler G, Hruban RH, Klöppel G. Intraductal papillary-mucinous neoplasms of the pancreas. In: Hamilton SR, Aaltonen LA, eds. Pathology and Genetics of Tumours of the Digestive System. WHO Classification of Tumours. Lyon, France: IARC Press, 2000:237-40. [ISBN 9789283224105]
Ohashi K, Murakami Y, Maruyama M. Four cases of mucin-producing cancer of the pancreas on specific findings of the papilla of Vater. Prog Dig Endosc 1982; 20:348-51.
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 2006; 6:17-32. [PMID 16327281]
Tanno S, Nakano Y, Nishikawa T, Nakamura K, Sasajima J, Minoguchi M, et al. Natural history of branch duct intraductal papillary-mucinous neoplasms of the pancreas without mural nodules: long-term follow-up results. Gut 2008; 57:339-43. [PMID 17660227]
Yamaguchi K, Ohuchida J, Ohtsuka T, Nakano K, Tanaka M. Intraductal papillary- mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas. Pancreatology 2002; 2:484-90. [PMID 12378117]
Kamisawa T, Tu Y, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Malignancies associated with intraductal papillary mucinous neoplasm of the pancreas. World J Gastroenterol 2005; 11:5688-90. [PMID 16237766]
Uehara H, Nakaizumi A, Ishikawa O, Iishi H, Tatsumi K, Takakura R, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut 2008; 57:1561-5. [PMID 18477671]
Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol 2007; 33:266-70. [PMID 17097848]
Kim BJ, Lee KT, Moon TG, Kang P, Lee JK, Kim JJ, et al. How do we interpret an elevated carbohydrate antigen 19-9 level in asymptomatic subjects? Dig Liver Dis 2009; 41:357-9. [PMID 19162573]
Yamazaki Y, Kubo K, Takamizawa A, Yamamoto H, Honda T, Sone S. Markers indicating deterioration of pulmonary Mycobacterium avium-intracelluare infection. Am J Respir Crit Care Med 1999; 160:1851-5. [PMID 10588596]
Watanabe K, Fujimura M, Kasahara K, Yasui M, Myou S, Watanabe A, Nakao S. Characteristic of pulmonary Mycobacterium avium-intracellulare complex (MAC) infection in comparison with those of tuberculosis. Respir Med 2003; 97:654-9. [PMID 12814150]
Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest 1992; 101:1605-9. [PMID 1600780]
Prince DS, Peterson DD, Steiner RM, Gottlieb JE, Scott R, Israel HL, et al. Infection with Mycobacterium avium complex in patients without predisposing conditions. N Engl J Med 1989; 321:863-8. [PMID 2770822]
Klöppel G, Solcia, E, Longnecker DS, CapellaC, Sobin LH. Histological Typing of Tumours of the Exocrine Pancreas (WHO. World Health Organization. International Histological Classification of Tumours). Berlin: Springer, 1996. [ISBN 3540602801]
Salvia R, Crippa S, Falconi M, Bassi C, Guarise A, Scarpa A, Pederzoli P. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut 2007; 56:1086-90. [PMID 17127707]
Rautou PE, Lévy P, Vullierme MP, O'Toole D, Couvelard A, Cazals-Hatem D, et al. Morphologic changes in branch duct intraductal papillary mucinous neoplasms of the pancreas: a midterm follow-up study. Clin Gastroenterol Hepatol 2008; 6:807-14. [PMID 18304885]
Pelaez-Luna M, Chari ST, Smyrk TC, Takahashi N, Clain JE, Levy MJ, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol 2007; 102:1759-64. [PMID 17686073]
Tang RS, Weinberg B, Dawson DW, Reber H, Hines OJ, Tomlinson JS, et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol 2008; 6:815-19. [PMID 18602036]
Nagai K, Doi R, Ito T, Kida A, Koizumi M, Masui T, et al. Single-institution of the international consensus guidelines for treatment of branch duct intraductal papillary mucinous neoplasms of the pancreas. J Hepatobiliary Pancreat Surg 2009:16:353-8. [PMID 19280108]
Sohn TA, Yeo CJ, Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Lillemoe KD. Intraductal papillary mucinous neoplasms of the pancreas: an increasingly recognized clinicopathologic entity. Ann Surg 2001; 234:313-22. [PMID 11524584]
Adsay NV. The "new kid on the block:" intraductal papillary mucinous neoplasms of the pancreas: current concepts and controversies. Surgery 2003; 133:459-63. [PMID 12773972]
Fritz S, Fernandez-del Castillo C, Mino-Kenudson M, Crippa S, Deshpande V, Lauwers GY, et al. Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals significant molecular differences compared to ductal adenocarcinom. Ann Surg 2009; 249:440-7. [PMID 19247032]
Weitz J, Buchler W. Branch intraductal papillary mucinous neoplasms: just the tip of the of the iceberg? Gut 2008; 57:1490-1. [PMID 18941002]
Azar C, Van de Stadt J, Rickaert F, Deviere J, Baize M, Klöppel G, et al. Intraductal papillary mucinous tumuors of the pancreas. Clinical and therapeutic issues in 32 patients. Gut 1996; 39:457-64. [PMID 8949654]
Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med 1997; 156:S1-25. [PMID 9279284]
Copyright (c) 2010 Vien X Nguyen, G Anton Decker, Ananya Das, M Edwyn Harrison, Alvin C Silva, Idris T Ocal, Joseph M Collins, Cuong C Nguyen

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.