Poor Compliance with ACG Guidelines for Nutrition and Antibiotics in the Management of Acute Pancreatitis: A North American Survey of Gastrointestinal Specialists and Primary Care Physicians
Abstract
Context Despite recent updates in the treatment of acute pancreatitis emphasizing enteral nutrition over parenteral nutrition as well as minimizing antibiotic usage, mortality rates from acute pancreatitis have not improved. Data has been limited regarding physician compliance to these guidelines in the United States. Methods A 20 question survey regarding practice patterns in the management of acute pancreatitis was distributed to physicians at multiple internal medicine and gastroenterology conferences in North America between 2009 and 2010. Responses were analyzed using the chi-square test and multivariate logistic regression. Results Out of 406 available respondents, 43.3% of physicians utilize total parenteral nutrition/peripheral parenteral nutrition (TPN/PPN) and 36.5% utilize nasojejunal (NJ) feedings. The preferred route of nutrition was significantly related to practice type (P<0.001): academic physicians were more likely to use NJ tube feeding than private practice physicians (52.1% vs. 19.9%) while private practitioners were more likely to utilize TPN/PPN than academic physicians (70.2% vs. 20.5%). Gastroenterologists and primary care physicians were equally non-compliant as both groups favored parenteral nutrition. Multivariate logistic regression demonstrated that practice type (P<0.001) was the only independent predictor of route of nutrition. Most survey respondents appropriately do not routinely utilize antibiotics for acute pancreatitis, but when antibiotics are initiated, they are for inappropriate indications such as fever and infection prophylaxis. Conclusions Many North American physicians are noncompliant with current ACG practice guidelines for the use of artificial nutrition in the management of acute pancreatitis, with overuse of TPN/PPN and underutilization of jejunal feedings. Antibiotics are initiated in acute pancreatitis for inappropriate indications, although there are conflicting recommendations for antibiotics in severe acute pancreatitis. Improved compliance with guidelines is needed to improve patient outcomes.
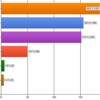
Image: The most common reasons cited for using parenteral nutrition.
Downloads
References
Swaroop VS, Chari ST, Clain JE. Severe acute pancreatitis. JAMA 2004; 291(23):2865-8. [PMID: 15199038].
Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas 2006; 33(4):323-30. [PMID: 17079934].
Banks PA, Freeman ML, Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006; 101(10):2379-400. PMID: [17032204].
McNaught CE, Woodcock NP, Mitchell CJ, Rowley G, Johnstone D, MacFie J. Gastric colonization, intestinal permeability and septic morbidity in acute pancreatitis. Pancreatology 2002; 2:463-8. [PMID: 12378114].
Ammouri BJ, Becker KL, Kite P, Snider RH, Nylen ES, White JC, et al. Calcitonin precursors: early markers of gut barrier dysfunction in patients with acute pancreatitis. Pancreas 2003 Oct; 27(3): 239-43. [PMID: 14508129].
Rahman SH, Ammori BJ, Holmfield JHM, et al. Intestinal hypoperfusion contributes to gut barrier failure in severe acute pancreatitis. J Gastrointest Surg. 2003; 7(1):26-35. [PMID: 12559182].
Ammori BJ, Barclay GR, Larvin M, McMahon MJ. Hypocalcemia in patients with acute pancreatitis: a putative role for systemic endotoxin exposure. Pancreas 2003; 26(3): 213-7. [PMID: 12657944].
Vu MK, van der Veek PP, Frolich M, Souverijn JH, Biemond I, Lamers CB, Masclee AA. Does jejunal feeding activate exocrine pancreatic secretion? Eur J Clin Invest. 1999; 29(12):1053-9. [PMID: 10583454].
Kaushik N, Pietraszewski M, Holst JJ, O’Keefe SJ. Enteral feeding without pancreatic stimulation. Pancreas 2005; 31(4):353-9. [PMID: 16258370].
Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surg Gynecol Obstet. 1993; 176(5):480-3. [PMID: 8480272].
Bassi C, Falconi M, Talamini G, Uomo G, Papaccio G, Dervenis C, et al. Controlled clinical trial of pefloxacin versus imipenem in severe acute pancreatitis. Gastroenterology 1998 Dec; 115(6): 1513-7. [PMID: 9834279].
Isenmann R, Rünzi M, Kron M, Kahl S, Kraus D, Jung N, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology 2004; 126(4):997-1004. [PMID: 15057739].
Norton SA, Cheruvu CV, Collins J, Dix FP, Eyre-Brook IA. An assessment of clinical guidelines for the management of acute pancreatitis. Ann R Coll Surg Engl. 2001; 83(6):399–405. [PMID: 11777135].
Chiang DT, Anozie A, Fleming WR, Kiroff GK. Comparative study on acute pancreatitis management. ANZ J Surg. 2004; 74(4):218–21. [PMID: 15043731].
Barnard J, Siriwardena AK. Variations in implementation of current national guidelines for the treatment of acute pancreatitis: implications for acute surgical service provision. Ann R Coll Surg Engl. 2002; 84(2):79–81. [PMID: 11995768].
Lankisch PG, Weber-Dany B, Lerch MM. Clinical perspectives in pancreatology: compliance with acute pancreatitis in Germany. Pancreatology 2005; 5(6):591–593. [PMID:16110257].
Bourque LB, Eve PF. How to Conduct Self-Administered and Mail Surveys. Thousand Oaks: Sage Publications, 2002.
Loveday BP, Srinivasa S, Vather R, Mittal A, Petrov MS, Phillips AR, Windsor JA. High quantity and variable quality of guidelines for acute pancreatitis: a systematic review. Am J Gastroenterol. 2010; 105(7): 1466-76. [PMID: 20606652].
Uhl W, Warshaw A, Imrie C, Bassi C, McKay CJ, Lankisch PG, Carter R, et al. IAP Guidelines for the Surgical Management of Acute Pancreatitis. Pancreatology. 2002; 2:565-573. [PMID: 15831893].
UK Working Party on Acute Pancreatitis. UK guidelines for the management of acute pancreatitis. Gut 2005; 54(Suppl 3): iii1–9. [PMID: 15831893].
Takeda K, Takada T, Kawarada Y, Hirata K, Mayumi T, Yoshida M, Sekimoto M, et al. JPN Guidelines for the management of acute pancreatitis: medical management of acute pancreatitis. J Hepatobiliary Pancreat Surg 2006;13:42–7. [PMID 16463210].
Kalfarentzos FE, Karavias DD, Karatzas TM, Alevizatos BA, Androulakis JA. Total parenteral nutrition in severe acute pancreatitis. J Am Coll Nutr. 1991; 10(2): 156-162. [PMID: 1903137].
Dejong CH, Greve JW. Nutrition in patients with acute pancreatitis. Curr Opin Crit Care 2001; 7(4): 251-6. [PMID: 11571422].
Al-Omran M, Groof A, Wilke D. Enteral versus parenteral nutrition of acute pancreatitis. Cochrane Database Syst Rev 2003; (1): CD002837. Update of: Cochrane Database Syst Rev. 2001; (2): CD002837. [PMID: 12535441].
Marik PE, Zaloga GP. Meta-analysis of parenteral nutrition versus enteral nutrition in patients with acute pancreatitis. BMJ. 2004; 328(7453):1407. [PMID:15175229].
Windsor AC, Kanwar S, Li AG, Barnes E, Guthrie JA, Spark JI, et al. Compared with parenteral nutrition, enteral feeding attenuates the acute phase response and improves disease severity in acute pancreatitis. Gut 1998; 42(3):431-435. [PMID: 9577354].
Papakostas C, Smailis D, Avgerinos C, Sofianou K, Lytras D, Kolibiris C, et al. Antibiotic prophylaxis in acute pancreatitis. Annals of Gastroenterology 2000; 13(4): 299-306.
Isenmann R, Rünzl M, Kron M, Kahl S, Kraus D, Jung N, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology 2004; 126(4):997-1004. [PMID: 15057739].
Mazaki T, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg. 2006; 93(6): 674-84. [PMID: 16703633].
García-Barrasa A, Borobia FG, Pallares R, Jorba R, Poves I, Busquets J, Fabreqat J. A double-blind, placebo-controlled trial of ciprofloxacin prophylaxis in patients with acute necrotizing pancreatitis. J Gastrointest Surg. 2009;13(4):768–74. [PMID 19082671].
Dellinger EP, Tellado JM, Soto NE, Ashley SW, Barie PS, Dugernier T, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Ann Surg. 2007; 245(5): 674–83. [PMID: 17457158].
Berild D, Ringertz SH, Lelek M, Fosse B. Antibiotic guidelines lead to reductions in the use and cost of antibiotics in a university hospital. Scand J Infect Dis. 2001; 33(1): 63-7. [PMID: 11234982].
Berzin T, Rocha F, Whang E, Mortele K, Ashley S, Banks P. Prevalence of primary fungal infections in necrotizing pancreatitis. Pancreatology 2007; 7(1): 63-6. [PMID: 17449967].
Forsmark CE, Baillie J, AGA Institute Clinical Practice and Economics Committee, AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology 2007; 132(5): 2022-44. [PMID: 17484894].
Copyright (c) 2014 Edward Sun, Mathew Tharakan, Sumit Kapoor, Rajarshi Chakravarty, Aladin Salhab, Jonathan M Buscaglia, Satish Nagula

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.