Total Pancreatectomy and Islet Auto-Transplantation as Treatment for Ampullary Adenocarcinoma in the Setting of Pancreatic Ductal Disruption Secondary to Acute Necrotizing Pancreatitis. A Case Report
Abstract
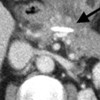
Context Ampullary adenocarcinoma is the third most common periampullary malignancy. Obstruction of the main pancreatic duct is linked with an increased incidence of acute pancreatitis. Acute necrotizing pancreatitis leading to pancreatic duct disruption carries significant morbidity. When these conditions occur in combination, the treatment can be drastically limited as pancreaticoduodenectomy is not a viable option in the setting of friable ductal tissue, which precludes pancreatic ductal anastomosis and can lead to the complications of leak or stricture. Case report Our patient is a 72-year-old woman who developed pancreatic ductal disruption and splenic vein thrombosis as a result of acute necrotizing pancreatitis. Concurrently, she was found to have an ampullary adenoma with high-grade dysplasia. Her treatment options were limited, as she was neither a candidate for pancreaticoduodenectomy given the ductal disruption nor total pancreatectomy, which would render her a brittle diabetic. She was successfully treated with total pancreatectomy and islet auto-transplantation thereby resecting her ampullary lesion while both avoiding a pancreatic anastomosis and preserving pancreatic endocrine beta-cell function. Conclusion We report a case where total pancreatectomy and islet auto-transplantation can be considered as a viable option for treatment of ampullary lesions in a setting where standard surgical options are suboptimal.
Downloads
References
Cameron JL, Cameron AM. Current Surgical Therapy, 10thEd. Philadelphia: Elsevier; 2011.
White SH, Nazarian NA, Smith AM, Balfour TW. Periampullary adenoma causing pancreatitis. Br Med J. 1981; 283(6290):527 [PMID 6790055]
Guzzardo G, Kleinman MS, Krackov JH, Schwartz SI. Recurrent acute pancreatitis caused by ampullary villous adenoma. J Clin Gastroenterol. 1990; 12(2):200-202 [PMID 2182707]
Van Esch AA, Drenth JP, te Morsche RH, Jansen JB, Nagengast FM. Recurrent idiopathic pancreatitis in familial adenomatous polyposis: a report of a case-series and review of the literature. Fam Cancer. 2007;6(3):275-280 [PMID 17318339]
Kim JH, Kim JH, Han JH, Yoo BM, Kim MW, Kim WH. Is endoscopic papillectomy safe for ampullary adenomas with high-grade dysplasia? Ann Surg Oncol. 2009; 16(9):2547-2554 [PMID 19568817]
Jung MK, Cho CM, Park SY, Jeon SW, Tak WY, Kweon YO, et al. Endoscopic resection of ampullary neoplasms: a single-center experience. Surg Endosc. 2009;23(11):2568-2574 [PMID 19360365]
Sutherland DE, Matas AJ, Najarian JS. Pancreatic islet cell transplantation. Surg Clin North Am. 1978;58(2):365-382 [PMID 418514]
Blondet JJ, Carlson AM, Kobayashi T, Jie T, Bellin M, Hering BJ, et al. The role of total pancreatectomy and islet autotransplantation for chronic pancreatitis. Surg Clin North Am. 2007;87(6):1477-1501 [PMID 18053843]
Sutherland DE, Gruessner AC, Carlson AM et al. Islet autotransplant outcomes after total pancreatectomy: a contrast to islet allograft outcomes. Transplantation. 2008;86(12):1799-1802 [PMID 19104425]
Liu X, Förster S, Adam U, Schmidt W, Müller P, Hopt UT. Islet autotransplantation combined with total pancreatectomy for treatment of pancreatic adenocarcinoma. Transplantation Proc. 2001;33(1-2):662-663 [PMID 11267005]
Förster S, Liu X, Adam U, Schareck WD, Hopt UT. Islet autotransplantation combined with pancreatectomy for treatment of pancreatic adenocarcinoma: a case report. Transplant Proc. 2004;36(4):1125-26 [PMID 15194392]
Alsaif F, Molinari M, Al-Masloom A, Lakey JR, Kin T, Shapiro AM. Pancreatic islet autotransplantation with completion pancreatectomy in the management of uncontrolled pancreatic fistula after whipple resection for ampullary adenocarcinoma. Pancreas. 2006;32(4):430-431 [PMID 16670628]
Lee BW, Jee JH, Heo JS, Choi SH, Jang KT, Noh JH, et al. The favorable outcome of human islet transplantation in Korea: experiences of 10 autologous transplantations. Transplantation. 2005;79(11):1568-1574 [PMID 15940047]
Copyright (c) 2014 Uroghupatei P Iyegha, Javariah A Asghar, Greg J Beilman

This work is licensed under a Creative Commons Attribution 4.0 International License.
As a member of Publisher International Linking Association, PILA, iMedPub Group’s JOP follows the Creative Commons Attribution License and Scholars Open Access publishing policies. Journal of the Pancreas is the Council Contributor Member of Council of Science Editors (CSE) and following the CSE slogan Education, Ethics, and Evidence for Editors.